Description
Buy HUCOG 1000 in USA without prescription
Chorionic Gonadotrophin Injection
Human chorionic gonadotropin (hCG) is a hormone produced by the placenta after implantation. The presence of hCG is detected in some pregnancy tests (HCG pregnancy strip tests). Some cancerous tumors produce this hormone; therefore, elevated levels measured when the patient is not pregnant can lead to a cancer diagnosis and, if high enough, paraneoplastic syndromes. However, it is not known whether this production is a contributing cause or an effect of carcinogenesis. The pituitary analog of hCG, known as luteinizing hormone (LH), is produced in the pituitary gland of males and females of all ages.
HCG INDICATIONS
Anovulatory infertility
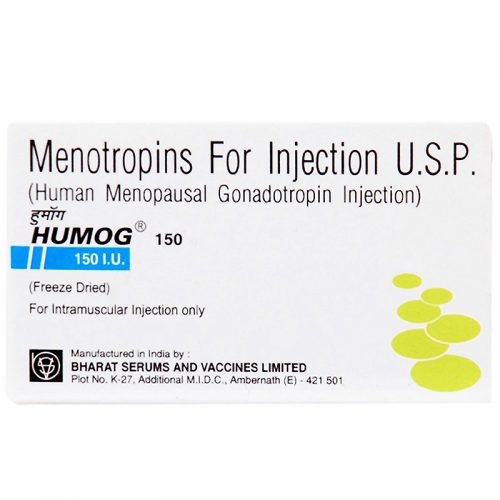
In the female, HUCOG is used in the treatment of anovulatory infertility. where its administration would form part of recognized treatment regimen involving prior stimulation of follicular maturation and endometrial proliferation e.q. with Menotropin Injection (HUMOG).
Firstly, follicle development is stimulated with daily injections of FSH or FSH and LH. Once the follicles have developed appropriately, one injection of HUCOG is given. The HCG in the HUCOG injection mimics the action of luteinising hormone and causes the release of an egg from the ovary. The woman is usually advised to have sex on the day of the HUCOG injection and the day after.
Hypogonadotrophin hypogonadism and cryptorchidism
In the male, HUCOG stimulates the interstitial cells of the testes and consequently the secretion of androgens and the development of secondary sexual characteristics. With concomitant Menotropin Injection therapy, HUCOG stimulates the induction and maintenance of spermatogenesis.
HCG DOSAGE AND ADMINISTRATION
HUCOG is given by subcutaneous / intramuscular injection only.
Anovulatory infertility
HUCOG 10000 I.U. is administered in mid-cycle, following treatment with Menotropin Injection (HUMOG) according to a recognised scheme.
Hypogonadotrophin hypogonadism and cryptorchidism
HUCOG 2000 I.U. twice weekly concomitant with Menotropin Injection (HUMOG) (1 vial three times a week) if necessary for a minimum period of four months.
Cryptorchidism
Equivalent to 1000 I.U. of HUCOG on alternate days for several weeks
Contra-Indication and Warnings
Stimulation of ovulation with HUCOG may lead to superovulation and the hyperstimulation syndrome. Oestrogen assays will detect the excessive response so that HUCOG (HCG) may be withheld in that particular treatment cycle. In the male, high dosages of HUCOG may lead to oedema and in such cases dosages should be considerably reduced.
If signs of sexual precocity are observed a reduced dosage regimen should be instituted.
Side Effects
Headache, irritability, restlessness, depression, fatigue, edema, gynecomastia, sexual precocity, pain at the site of injection.
Adverse Events
The adverse reactions for use in infertility are:
- Ovarian hyperstimulation (OHSS), a syndrome of sudden ovarian enlargement, ascites with or without pain, and/or pleural effusion
- Rupture of ovarian cysts with resultant hemoperitoneum
- Multiple births
- Arterial thrombo-embolism
PRECAUTION
Please, read article “Fertility treatment with hCG injections” before hCG Injection use.
HCG should be used in conjunction with human menopausal gonadotropins only by physicians experienced with infertility problems who are familiar with the criteria for patient selection, contraindications, warnings, precautions, and adverse reactions described in the package insert for menotropins.
Interaction with other medicinal products and other forms of interaction
Concomitant use of HuCoG Injection with other agents used to stimulate ovulation (e.g. HMG, clomiphene citrate) may potentiate the follicular response. (See Warnings Precaution & Overdosage.)
Overdose
The effects of an overdose of HuCoG Injection are unknown, nevertheless one could expect ovarian hyperstimulation syndrome (OHSS) to occur, which is further described as below:
Ovarian Hyperstimulation Syndrome (OHSS)
OHSS is a medical event distinct from uncomplicated ovarian enlargement. OHSS is a syndrome that can manifest itself with increasing degrees of severity. It comprises marked ovarian enlargement, high serum sex steroids, and an increase in vascular permeability which can result in an accumulation of fluid in the peritoneal, pleural and, rarely, in the pericardial cavities.
The following symptomatology may be observed in severe cases of OHSS: abdominal pain, abdominal distension, severe ovarian enlargement, weight gain, dyspnoea, oliguria and gastrointestinal symptoms including nausea, vomiting and diarrhoea.
Adherence to recommended HuCoG Injection dosage, regimen of administration and careful monitoring of therapy will minimize the incidence of ovarian hyper stimulation and multiple gestations. In ART, aspiration of all follicles prior to ovulation may reduce the occurrence of hyper stimulation. OHSS may be more severe and more protracted if pregnancy occurs. Most often, OHSS occurs after hormonal treatment has been discontinued and reaches its maximum at about seven to ten days following treatment. Usually, OHSS resolves spontaneously with the onset of menses. If severe OHSS occurs, gonadotrophin treatment should be stopped if still ongoing, the patient hospitalized and specific therapy for OHSS started. This syndrome occurs with higher incidence in patients with polycystic ovarian disease.
Ovarian response should be carefully monitored to minimize the risk of overstimulation. If the ovaries are abnormally enlarged on last day of gonadotrophin therapy, HCG should not to be administered in this course therapy. This reduces development of OHSS (Ovarian Hyperstimulation Syndrome). Use of ultrasound monitoring of ovarian response and/or measurement of serum estradiol levels can further minimize the risk of overstimulation.
Storage
Vials of HUCOG should be stored between 20C-80C. Do not freeze. Protect from light. Any unused portion should be discarded.
PRESENTATION
HUCOG is supplied in vials containing sterile having activity of 10000 I.U.



Reviews
There are no reviews yet.